3 Reasons Why a Young Person May Need a Colonoscopy
A colonoscopy is a medical procedure that allows your gastroenterologist to examine the large bowel for abnormalities. The physician carefully inserts the colonoscope, a flexible tube with a digital camera and light at the end, into the anus to get a better look inside of the colon. A monitor connected to the colonoscope displays a magnified live feed view of the colon lining. Traditionally, colonoscopies are for adults over the age of 50, but young adults may also need this procedure as well. It is never a bad idea to consult a gastroenterologist and ask for one if you are experiencing symptoms that concern you. Here are 3 reasons why a young person may need a colonoscopy.
Rising Cancer Rates in Young Adults
Colonoscopies serve two major purposes: detection and diagnosis. Typically, adults over the age of 50 have a colonoscopy to proactively screen for signs of cancer. Colon polyps are growths on the lining of the colon that can sometimes become cancerous. During a colonoscopy, doctors will remove any potentially cancerous polyps to prevent further growth. If a young adult experiences symptoms of colorectal cancer, they should talk to their doctor, and if no clear cause of the symptoms is found, a diagnostic colonoscopy may be in order. This procedure will identify the cause of symptoms so that if cancer is present, it can be treated as early as possible. Colonoscopies are used as a screening method for colorectal cancer starting at age 45 (based on recommendations from the American Cancer Society) but may be used to screen for cancer in those younger than 45 if they have a family history of the disease. Colorectal cancer rates are rising among millennials and Gen Xers, but the fatality rate for colorectal cancer has steadily decreased over the past couple of decades for reasons doctors are partially attributing to better screening of young adults.
Proper Diagnosis
Discussing bathroom habits with your doctor may be uncomfortable for some, but only giving vague descriptions of symptoms makes properly diagnosing the problem more challenging. These various irritable bowel diseases have symptoms that overlap, and doctors need concrete evidence to diagnose you and offer proper treatment.
Crohn’s Disease
Crohn’s disease is part of a group of digestive conditions called inflammatory bowel disease (IBD). This autoimmune disease causes inflammation to occur in sections of the large and small intestines. The inflammation is the result of the body’s immune system recognizing the cells in the digestive tract as foreign and attacking them. While doctors are still not sure what causes the disease, genetics and family history are thought to play a part. The most common symptoms of Crohn’s disease are abdominal pain, weight loss, diarrhea, fever, and rectal bleeding.
Ulcerative Colitis
Ulcerative colitis is another inflammatory bowel disease that affects as many as 907,000 Americans. The symptoms of ulcerative colitis are very similar to those of Crohn’s, but the part of the digestive tract affected by colitis is solely the large intestine. Shared symptoms include abdominal pain and cramping, bloody stool, reduced appetite, diarrhea, fatigue, fever, and unintended weight loss. Eliminating foods that cause discomfort and taking medication can help to suppress the inflammation caused by ulcerative colitis.
Irritable Bowel Syndrome
An estimated 10% of people worldwide suffer from Irritable bowel syndrome (IBS), a chronic disorder of the large intestine. With IBS, muscles in the colon may contract strongly, resulting in bloating, gas, and diarrhea, or contract weakly, slowing the passage of food and causing a hard stool. Unlike inflammatory bowel diseases, such as ulcerative colitis or Crohn’s disease, IBS does not result in changes in bowel tissue or increase the risk of developing colorectal cancer. What causes IBS is not known, however, its treatment plan centers largely on dieting decisions, such as eating low-fat, high-fiber meals or avoiding common trigger foods. Stress can also trigger IBS symptoms. Some people find cognitive-behavioral therapy or low-dose antidepressants to be useful treatments as well.
Preventative Screening
Just because you have not experienced any noticeable symptoms, that does not necessarily mean that everything is functioning normally. A sudden and consistent change in bowel movements and rectal pain and bleeding are the most common symptoms, but some people will not notice any changes until the cancer’s late stages. The best way to prevent colorectal cancer is regular visits with your doctor, and making sure that you get screened at recommended intervals beginning between ages 45 and 50. As with all cancers, the sooner colorectal cancer is diagnosed, the better the chance a person will live a longer and healthier life.
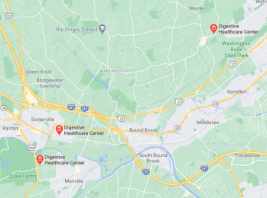
Colonoscopies and Digestive Healthcare in New Jersey
Colonoscopies are not as scary as they are often made out to be. If you or someone you know has been experiencing persistent stomach pain or has a family history of colon cancer, consider giving the qualified staff at Digestive Healthcare Center a call. Our doctors will examine you, taking into account your medical history and symptoms, and arrange an individualized treatment program if further testing is needed. We offer a number of procedures, all focused on staying on top of your digestive health. For more information about colonoscopies, colon cancer, or general digestive health, contact us at 862-217-5141 today!
Make an Appointment for Comprehensive Digestive Care in NJ
At Digestive Healthcare Center, we want each patient at our three offices in New Jersey to feel confident about their digestive health. We encourage you to contact us today to make an appointment with one of our expert gastroenterologists – don’t wait to start putting your digestive health first!
Recent Blogs
Learn more about all things digestive health and wellness by checking out our recent gastroenterology blogs.

Diverticular disease and diverticulitis are related digestive health conditions that affect the large intestine (colon). With diverticular disease, small, bulging pockets develop on the lining of the colon. When these pockets become inflamed or infected, the condition is called diverticulitis. They are very common – especially after age 40 – and rarely cause problems. At […]

Many Americans like to set New Year’s resolutions to make positive lifestyle changes such as improving their diet and going to the gym. However, March is also a great time for a healthy focus, especially as the long winter season comes to an end. National Nutrition Month, sponsored by the Academy of Nutrition and Dietetics, […]

Gallstones form when bile stored in the gallbladder hardens. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. It holds a digestive fluid called bile that’s released into your small intestine. Gallstones are pebble-like pieces of concentrated bile material, typically made up of cholesterol or bilirubin […]